In this guide, we are going to talk about, and give examples on how to write Progress and Shift notes that aim to support the client’s goals and record information relevant to the events that occur on shift.
The information you write in progress and shift notes frequently crosses over. This is because Progress notes record the progress a client makes with their goals, and Shift notes record what occurs on a shift.
Most teams use a book or app that records both progress and shift notes in one document. Independent support workers can keep their own shift and progress notes for the client, but they must be kept in a secure location when not on shift.
What should your care notes do?
A care record should simply document what you Do, See, and Hear.
Care records should not contain the writer’s opinions, personal feelings, assumptions, speculation, or judgements.
Interpretations may be included, but they must be
accompanied by solid evidence as to why they were made.
For example, you can write. “Andy appeared to be frustrated and angry at the park today after not being able to go on the swings as other children were using them. He stomped his foot 5 times and he paced in front of the swings.” Here, you are interpreting Andy’s emotion because you can’t actually know what he is feeling.
FACT Criteria
Use the F.A.C.T. criteria to improve your documentation.
Factual
- Be specific
- Use neutral language
- Avoid bias and assumptions
- Record information you see, hear, or otherwise observe through your senses.
Neutral language can feel clinical and impersonal when writing notes on a client that you have developed a relationship with. It’s important to use neutral language to avoid casual and unprofessional writing.
One of the most common errors in notes is writing judgements and not facts e.g: Chris ate well, Justine slept well. These notes are lazy and fail to describe facts. Examples of factual statements are: “Justine slept for 6 hours.”. “Chris ate all of his dinner.”
Recording errors factually
Written record keeping errors cannot be erased, whited out or otherwise made illegible. The error should be dealt with by drawing a line through the text and writing “error” with your initials.
For example:
Accurate
Be precise. State times, amounts, weight, size, units and measurements e.g.
"John hit his head with his hand 3 times."
"Gordon spent 4.65 hours on community access today."
"Janey drank 800ml of water today."
Complete
Complete your notes for legal purposes:
- Write ‘n/a’ where a question or section does not apply. For example, incident reports, behaviour charts and other care forms.
- Always sign on and off, stating time and date.
- Include the clients name, address or NDIS no. on each page if you are writing in a book that does not have page numbers.
- There should be no blank spaces in your shift notes. This protects you from claims by a court that information was added to the notes after the fact. After sign off, always draw a line to the end of the row or page to prevent additions.
- If you need to add information that you forgot from a previous shift, write it up on a separate page, noting that it is additional information. Include the time and date that you have written the additional information.
- Continued notes – If care notes run over two or more pages, a notation that the entry is ‘cont. on next page’ must be made to indicate that the care notes are incomplete.
Time Based
When a medical record is examined in court, date and times are critical. It establishes timely response to a client need and proof of the appropriate care provided.
Many healthcare institutions now use a 24-hour clock to lessen error. Midnight is recorded as 24:00 and the start of the day is 00:00. These are the exact same times so you can use either if your shift crosses midnight. Please be consistent.
If your written entry refers to events earlier in the shift, be sure you note the time you are talking about.
What to document?
Activities you need to document are
- baths and daily hygiene, skin care
- repositioning and turning
- bed changes
- equipment usage
- wound care
- use of incontinence pads
- range of motion issues
- exercise
- community access activities
- visits to therapist or doctor
You should also observe and record
- changes in client’s awareness and mental states
- unusual behaviours
- vital signs if needed
- urinary and bowel motions
- skin colour and warmth
- sleep cycles
- meal and fluid intake
- reactions to medication or foods
Generally include in your care notes
- use of speech communication devices and/or therapy equipment
- medication assistance (a separate Medication Chart is recommended)
- incidents, accidents and hazards (a separate Incident Form and/or Hazard Report is recommended)
- daily living tasks such as cleaning and food preparation
- notes on progress the client is making relevant to their goals
- any other factual observations you may feel are relevant
Always include unusual physical or emotional changes or reactions. If a client passes away or has a major medical incident whilst in your care, this information will be significant.
Always write notes if someone specifically directed you to do a task or activity in the daily care you provide; for example, a client, family member, or your supervisor. If the task has negative consequences, you will have evidence of direction, however, use your judgement here and follow your duty of care obligations.
Not all of the above will be relevant to a specific client. It is simply a broad list of care components that can be documented.
How to document?
If hand entries are used, then writing should be done with a blue or black permanent ink pen. Writing should be neat and legible. Use block printing if your handwriting is poor.
Some facilities only allow the use of black pen. If you are part of a care team, ask your supervisor or team leader if there is a preference.
White spaces – NO white spaces should be left on care records. Eliminating white spaces by drawing a line through them prevents additions to your records by other people. Yes, this is more work, however it means you will be protected from fraud and from claims in court that your notes are not legally compliant.
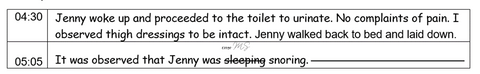
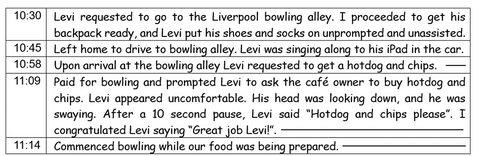
Narrative documentation – Many support workers feel comfortable with this style. Narrative documentation provides a running chronological report of the client’s care, activities and responses over the course of a shift. An example of this style is as follows:
Maintain Security and Confidentiality
Support workers are personally accountable for taking reasonable steps to ensure all client information is maintained in a secure and safe manner. The collection, handling and storage of a client’s personal and sensitive information is regulated under the Privacy Act 1988 (Cth).
Consider for example that you left your shift notes book in your car overnight and the vehicle was stolen. The client can sue you for breach of the Privacy Act as the book was not stored in a safe manner and their private details –their name, address, phone number, and personal care requirements, daily schedule, etc – are now in someone else’s hands. When not on shift, reasonable steps to secure your files include storing them at the client's home or in a locked case in your car or in a filing cabinet.
If your client requests to see the care records you maintain, that is their right. Please maintain a separate progress notes book or file for each client to avoid client’s viewing another person’s records.
All care records must for legal reasons be maintained for a minimum of 7 years from separation.
Happy record keeping!